Aged Care Regulation: Understanding the Strengthened Aged Care Quality Standards
Overview
In 2021, the Royal Commission into Aged Care Quality and Safety recommended a revision of the Aged Care Quality Standards, emphasising the need for them to better cover critical areas such as food, dementia, governance, and clinical care. In response, the Department of Health and Aged Care has developed the Strengthened Quality Standards. The refined Standards, currently in draft, align with the proposed new In-Home Aged Care Program, which is anticipated to commence from July 1, 2024.
The recent Consultation Paper on the New Regulatory Model for Aged Care, which we covered in a previous post, provides insight into how the strengthened Standards would apply across various service types, and outlines current thoughts on the future reform journey. To complement this, and support the sector to implement the Standards and associated regulatory reforms, the Aged Care Quality and Safety Commission has released a Framework Analysis detailing the proposed changes to the Quality Standards.
The rest of this article sets out the key changes to the Quality Standards. It is important to note that the Standards are currently being piloted with 40 providers across the country, which means the Standards may be revised further following the pilot. For a detailed overview of the changes to each Standard, their Outcomes, and Actions, see the Framework Analysis.
The Strengthened Quality Standards
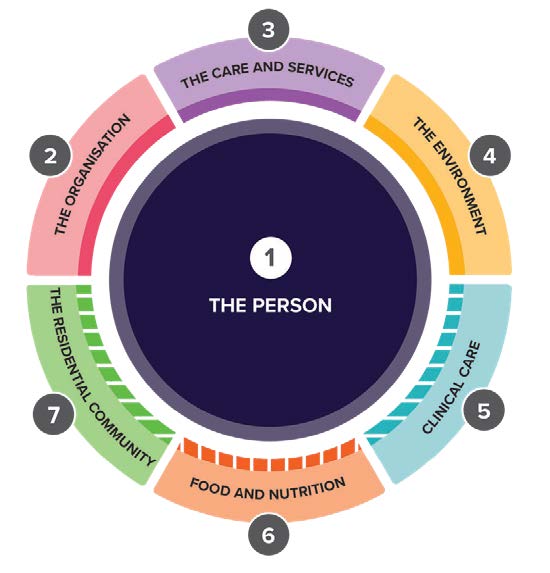
The number of Standards has been reduced from eight to seven, each serving a distinct purpose:
- Standard 1 (The Person): Promotes respect, individuality and diversity, independence, choice and control, and culturally safe care for older people.
- Standard 2 (The Organisation): Holds the governing body accountable for delivering quality care and services in compliance with the Standards.
- Standard 3 (The Care and Services): Describes how care and services should be provided across all service types.
- Standard 4 (The Environment): Ensures safe, supportive environments that cater to the needs of older people.
- Standard 5 (Clinical Care): Defines providers’ responsibilities to deliver safe, high-quality clinical care to the elderly.
- Standard 6 (Food and Nutrition): Encourages engaging with older people regarding their food preferences, delivering choice, and providing flavourful, appealing, and nutritious meals.
- Standard 7 (The Residential Community): Aims to optimise quality of life for older people in residential settings, by promoting the use of their skills and strengths and enabling them to engage in activities they enjoy.
Source: Aged Care Quality and Safety Commission, June 2023, Strengthened Quality Standards Framework Analysis, ACQSC, Australian Government.
The revised Standards use language that prioritises outcomes for older people, especially in terms of choice, inclusion, and quality of life. A total of 137 Actions underpin the Standards, to assist providers and staff achieve these outcomes. Of these 137 Actions:
- 21 align with existing Standard requirements
- 16 align with other existing legislative provider obligations
- 93 clarify existing requirements in the current Standards and
- 22 introduce new concepts or enhanced expectations.
Key Changes
The Actions that introduce new concepts or enhanced expectations relate to:
- Standard 2 (the Organisation)
- Standard 3 (the Care and Services)
- Standard 5 (Clinical Care) and
- Standard 6 (Food and Nutrition).
These are summarised below.
Standard 2 - The Organisation
Outcome 2.2 Quality and Safety Culture
Action 2.2.2: Enhanced requirements for governing bodies:
- for strategic and business planning and
- to address, through strategies and business planning, access issues for First Nations people and older people living with dementia.
Outcome 2.3 Accountability and Quality System
- Action 2.3.2: Enhanced requirement for governing bodies to ensure investments in priority areas deliver improved outcomes for older people.
- Action 2.3.4: New requirement for providers to regularly report on their quality system and performance to older people, families, and carers.
Outcome 2.8 Workforce Planning
- Action 2.8.2: Enhanced requirement for providers to support and maintain a satisfied and psychologically safe workforce.
Outcome 2.10 Emergency and Disaster Management
- Action 2.10.3: New requirement for providers to undertake emergency and disaster management planning that includes engagement with older people, families, carers, and workers.
- Action 2.10.4: New requirement for regular testing and review of emergency and disaster management plans.
Standard 3 - the Care and Services
Outcome 3.2 Delivery of Care Services
- Action 3.2.6: Enhanced requirement for providers to have a system to identify and review the skills and strengths of people living with dementia and encourage their use on a day-to-day basis.
Outcome 3.3 Communicating for Safety and Quality
Action 3.3.4: Enhanced requirements for providers to:
- identify and match older people to their care and services and
- provide monthly care statements.
Standard 5 - Clinical Care
Outcome 5.1 Clinical Governance
- Action 5.1.3: Enhanced requirement for providers to implement processes to ensure clinical care is trauma aware and healing informed.
- Action 5.1.5: New requirement for providers and health professionals to agree on their respective roles, responsibilities, and protocols for providing clinical care. This is not included in the scope of the existing Standard 8 (which covers clinical governance).
- Action 5.1.6: New requirement for providers to work towards implementing a digital clinical information system.
Outcome 5.3 Safe and Quality Use of Medicines
- Action 5.3.2: New requirement for providers to ensure relevant health professionals review, plan, and make changes to medicines for older people when they are acutely unwell.
- Action 5.3.3: Enhanced requirement for providers to have processes in place to ensure medication reviews are conducted, that includes actions or events that indicate when these must occur.
- Action 5.3.6: New requirement for providers to report adverse medicine and vaccine events to the Therapeutic Goods Administration.
- Action 5.3.7: Enhanced requirement for providers to regularly review and improve the effectiveness of systems for the safe and quality use of medicines.
Outcome 5.5 Clinical Safety
- Action 5.5.6: Enhanced requirement for providers to maintain older people’s oral health and prevent decline, including through assessing, monitoring, reviewing, and responding to oral health needs, and assistance with daily oral hygiene needs.
Standard 6 - Food and Nutrition
Outcome 6.1 Partnering with Older People on Food and Nutrition
- Action 6.1.1: Enhanced requirement for providers to partner with older people on how to create an enjoyable food, drink, and dining experience.
- Action 6.2.2: Enhanced requirement for providers to monitor and continuously improve their food services in response to older people’s satisfaction and intake, impact on health outcomes, and contemporary evidence-based practice.
Outcome 6.3 Provision of Food and Drink
- Action 6.3.1: Enhanced requirement to develop and review menus in partnership with older people and relevant health professionals.
- Action 6.3.2: Enhanced requirement for older people to exercise choice about what, when, where, and how they eat and drink.
- Action 6.3.4: Enhanced requirement for providers to offer and enable access to nutritious snacks and drinks (including water) at all times.
Outcome 6.4 Dining Experience
- Action 6.4.3: New requirement for providers to ensure there are opportunities for older people to share food and drinks with their visitors.
Provider Institute Best Practice Tip
The application of the revised Quality Standards will be like that of the NDIS Practice Standards, where certain Standards apply to providers depending on the services they deliver. All providers subject to the Quality Standards will be expected to demonstrate compliance with Standards One to Four. Providers delivering certain service types will also be required to demonstrate compliance with Standards Five, Six, and/or Seven. While the Standards will not be introduced formally until 2024, we strongly encourage providers to start preparing now by:
- reviewing our previous post on the new regulatory model for Aged Care
- determining which Registration Categories will apply to your organisation based on the services you deliver, or intend to deliver and
- understanding the expectations of the revised Quality Standards that will apply to your service delivery.
We recommend focusing on how the strengthened Standards will impact your organisation’s governance, quality management system (including its policies and procedures), workforce management, and service delivery. Training and communication with staff will be essential, as will clear communication with older people and their families on the changes and how they will impact them. Also consider any implications if you deliver other services that are required to meet quality standards, such as NDIS services.
If you’re not already, become a member of the Provider Institute of Australia to keep across these important changes as they develop, and to stay compliant with regulatory requirements as they also continue to evolve.
